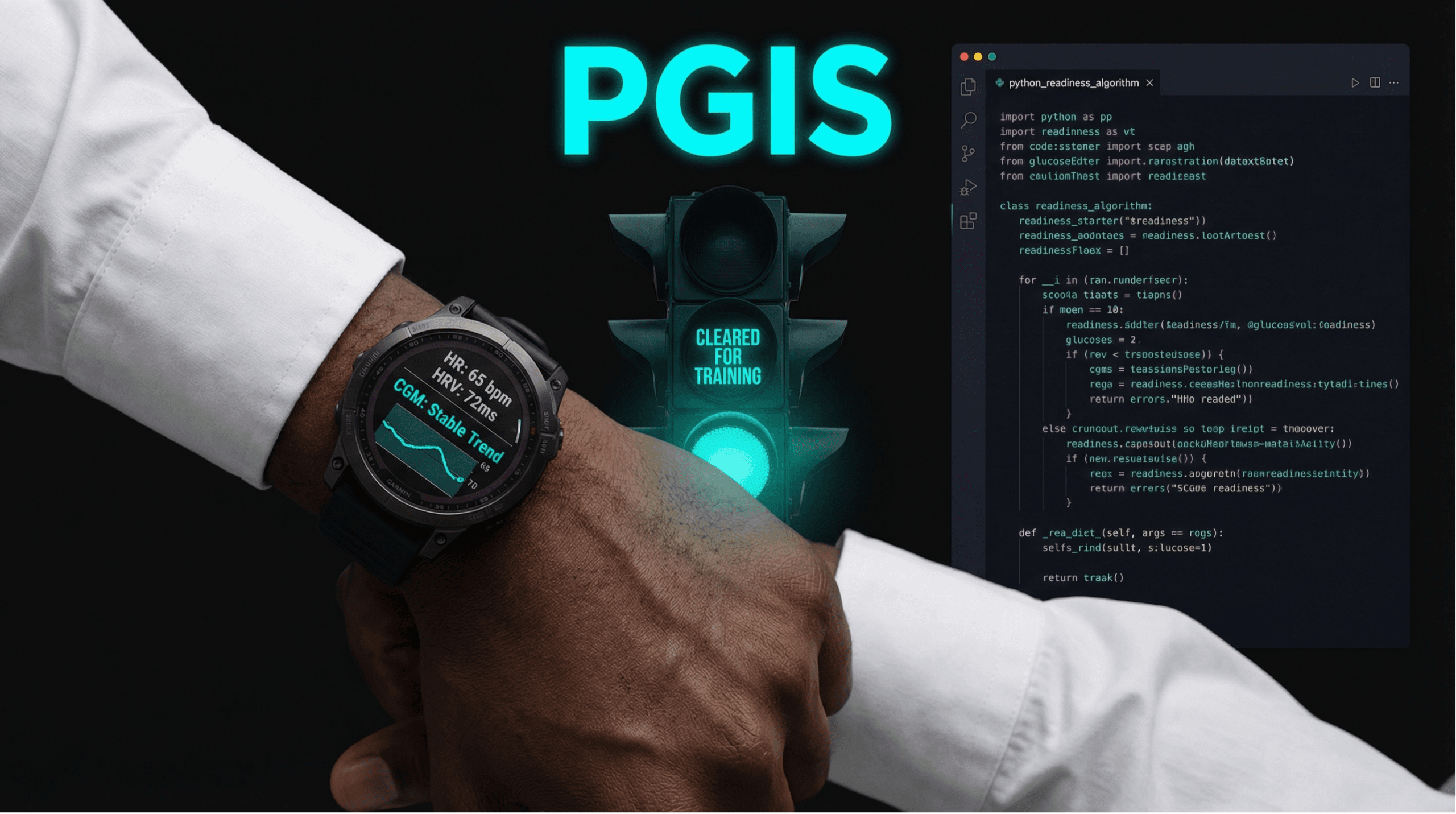
From Patient Data to Open Source: Why I Built the Performance Glycemic Intelligence System (PGIS)
As a physician-developer and a 60-year-old endurance athlete living with Type 2 diabetes for over two decades, I have navigated a unique intersection of medicine, technology, and personal health. My journey is a constant balancing act between the drive for athletic performance and the non-negotiable demands of glycemic control. This personal challenge is the crucible […]